Practice Consideration
Pathophysiology of Non-IgE-mediated Food Allergy
Non-IgE-mediated food allergies are characterized by a delayed reaction to specific food antigens that does not involve immunoglobulin E. The precise pathophysiological mechanisms underlying these reactions remain unclear. However, they are hypothesized to involve complex processes such as cell signaling, inflammatory cytokines and migration of cells to the site.(1)
Non-IgE-mediated allergies generally involve delayed onset symptoms, predominantly affecting the gastrointestinal tract. They are most commonly observed in pediatric patients, and tend to resolve as the child matures. In contrast to IgE-mediated reactions, which trigger a rapid release of histamines, non-IgE-mediated allergies instead involve a cellular immune response. The clinical manifestations of non-IgE-mediated food allergies typically emerge more than two hours after the ingestions of the allergen and are primarily gastrointestinal.
Symptoms include frequent and/or loose stools, the presence of blood and/or mucus in stools, abdominal pain, vomiting, food refusal or aversion. Additional symptoms may include atopic dermatitis or eczema and faltering growth, highlighting the broader systemic impact of these immune responses.
Diagnosis is more challenging and involves dietary exclusion and rechallenge.
Non-IgE-mediated Cow’s Milk Allergy
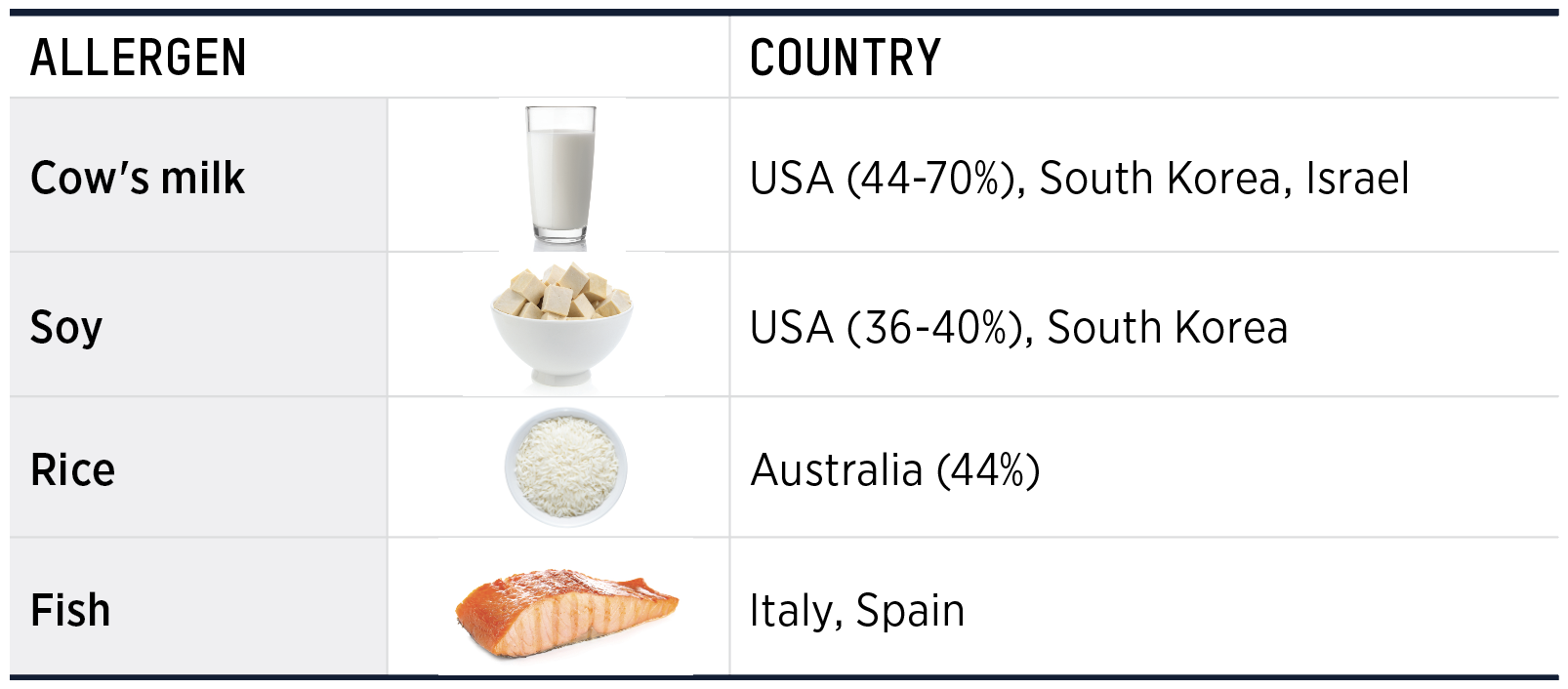
Non-IgE-mediated Co's Milk Allergy is common in infancy and early childhood and usually resolves by 3 to 5 years of age. It is associated with a broad range of symptoms ranging from mild symptoms of mucous and blood in stools in allergic proctocolitis to severe vomiting and collapse in food protein induced enterocolitis (FPIES).(2) The following are different types of non-IgE cow's milk allergy. The characteristics of each are listed in Table 1.1.
- Food protein-induced allergic proctocolitis (FPIAP)
- Food protein-induced enterocolitis (FPE)
- Food protein-induced enterocolitis syndrome (FPIES)
- Eosinophilic Esophagitis (EoE)
TABLE 1.1 Characterisitics of FPIAP, FPE, FPIES(Adapted from 2)
 |
1. Food protein-induced allergic proctocolitis (FPIAP)
FPIAP is a non-IgE-mediated food allergy commonly seen in otherwise healthy, thriving infants. It presents at about 2 to 8 weeks of age.(2) It is characterized by the presence of blood-streaked stools and mucus in otherwise healthy, thriving infants. It is often associated with the ingestion of cow's milk or soy protein. The condition is generally mild, and most infants outgrow FPIAP by their first year. Diagnosis is based on clinical presentation and improvement following the removal of the offending protein in the diet.
2. Food protein-induced Enterocolitis Syndrome (FPIES)
FPIES is an uncommon, non-IgE-mediated food allergy characterized by severe vomiting, lethargy and, in some cases, diarrhea following the ingestion of specific proteins. It occurs in older infants or young children around the time of solid food introduction. The onset of symptoms typically occurs within hours of consuming the trigger food.
Several phenotypes of FPIES have been described, including acute FPIES and chronic FPIES.(3)
Acute FPIES
Symptoms of acute FPIES include repetitive, profuse vomiting 1-4 hours after ingestion of the causal food. Often the infant becomes pale and lethargic or floppy and may have diarrhoea 5-10 hours after ingestion. There are no skin or respiratory symptoms.
Chronic FPIES
Chronic FPIES, is associated with poor growth and chronic diarrhea. It occurs in infants younger than 12 months. Symptoms resolve within 24 hours and infants and children are well unless exposure to the causal food occurs. Adrenaline is not effective in treating FPIES.(10) Symptoms and management are similar to those of non-IgE-mediated allergy, such as food protein-induced enteropathy(4)
3. Food protein-induced enterocolitis (FPE)
Characterized by malabsorption, faltering growth, anemia, diarrhea and vomiting in infants under 9 months of age.(2)
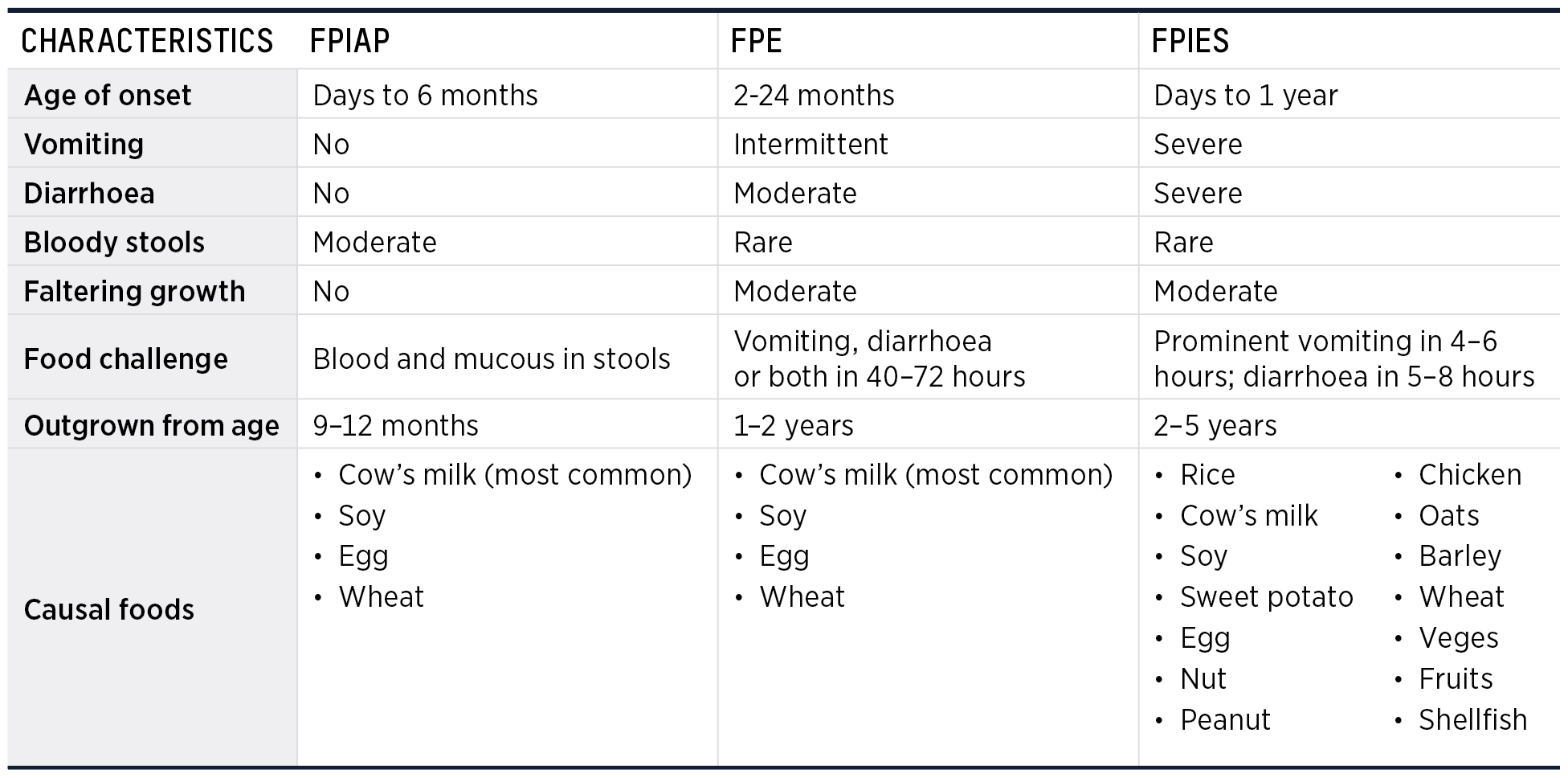
Foods Associated with FPIES
There is a wide range of foods that trigger FPIES including rice, cow’s milk, soy, sweet potato, egg, chicken, some vegetables and fruits. Trigger foods vary by geographical location. The following table outlines major food triggers by country and prevalence.(3)
TABLE 1.2 FPIES triggers by geographical location(3)
|
NB In Israel there is no soy FPIES or soy formula. |
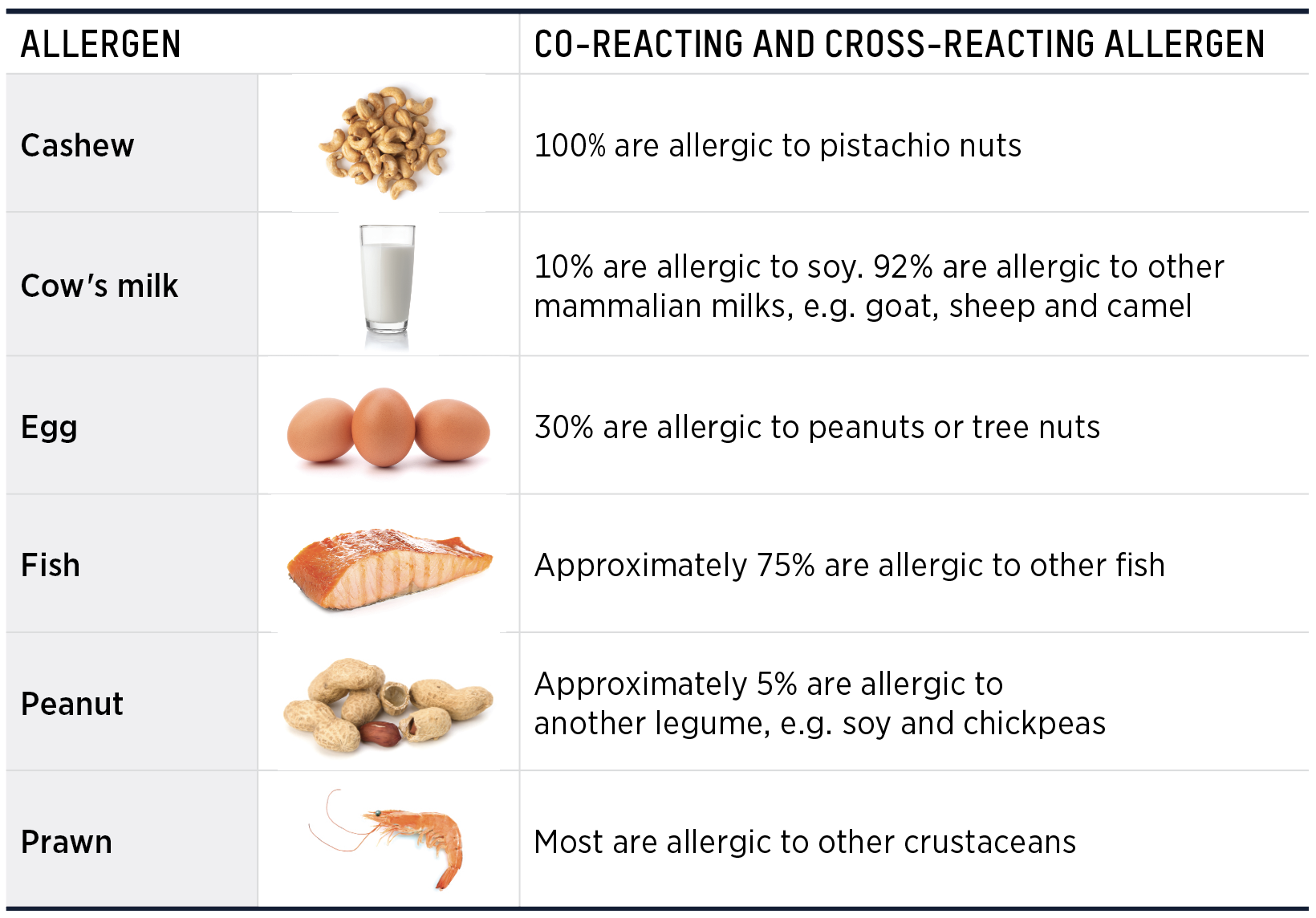
Most infants react to a single food but 15–35% react to two or more foods. Reaction to one food may increase risk of reaction to others in that food group (see Table 7.5.7 below).(3,5)
TABLE 1.3 Causal and co-reacting foods in FPIES(3)
 |
Feeding Skill Development
FPIES is associated with oral food aversion and poor feeding skill development, especially when three or more foods are trigger foods.(3) Food restriction and anxiety associated with risk of FPIES,
can negatively impact on mealtime structure and feeding interaction with caregiver, in addition to reducing variety.(3)
Cow’s milk is a very good source of high-quality protein, fat, easily assimilated calcium and riboflavin and it has significant levels of vitamin B12, vitamin A, vitamin D, magnesium and phosphate. Cow’s milk exclusion diets can have detrimental effects on growth and development if milk is not adequately substituted. Dietary education must include other names for cow's milk which may be listed under ingredients on the packaging of processed foods.
Suitable specialised infant formula for cow's milk allergy
Table 1.4 describes specialised infant formula suitable for cow's milk allergy and indicates which are appropriate in infants and children who need to avoid cow’s milk protein. Further information is available on www.allergy.org.au
TABLE 1.4 Specialised infant formula suitable for cow's milk allergy (CMA)
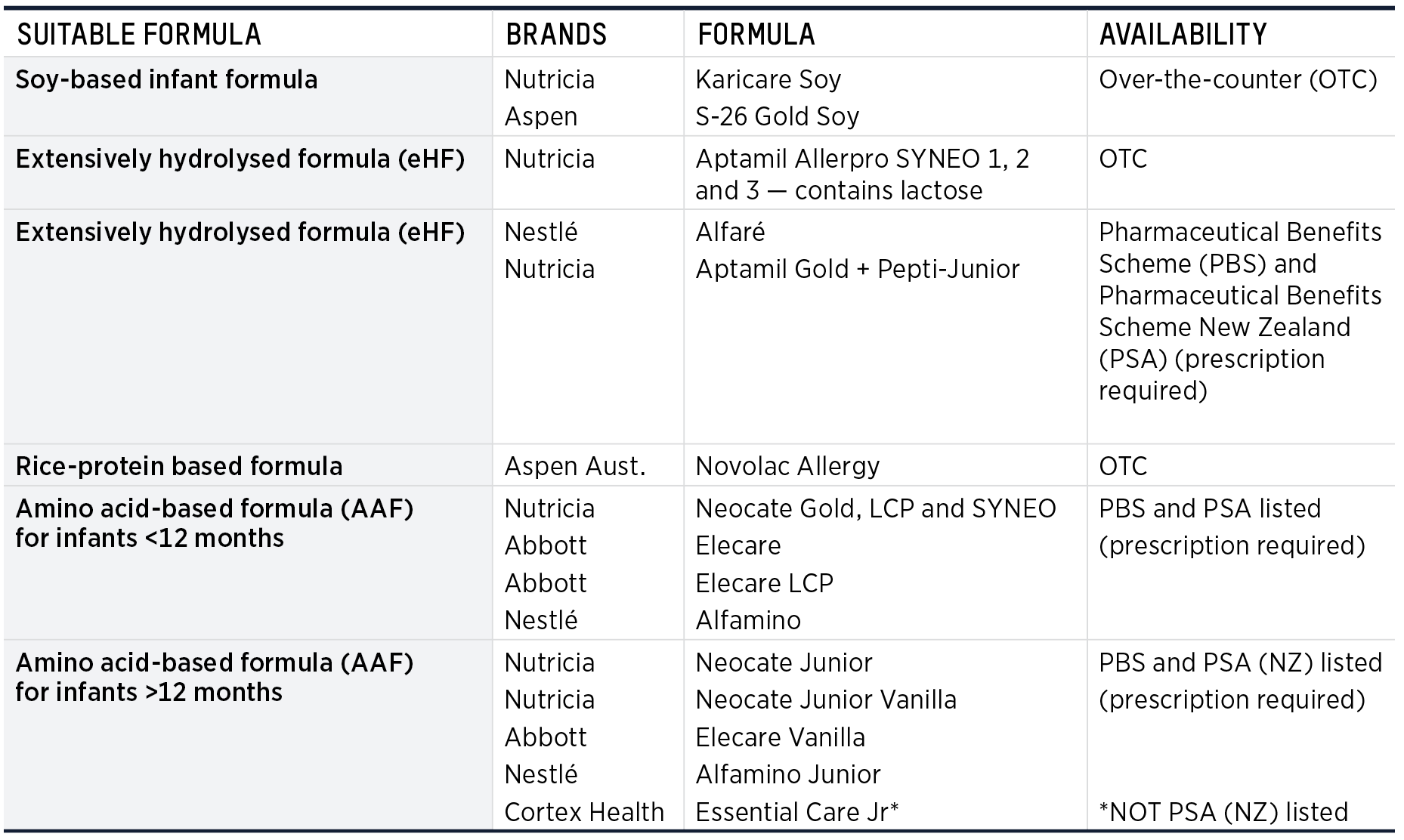 |
Infant Formula NOT Recommended for CMA
The following types of formula are NOT recommended for infants with CMA:
- Standard infant formula including anti-regurgitation, lactose-free, organic, newborn, and follow-on
- Goat milk-based infant formula
- Other mammal milks and formula
- A2 formula
NB For children with cow’s milk and soy allergies, most plant-based milk replacement products that are not fortified with calcium are too low in protein, fat, and calcium. They are not nutritionally adequate for children <2 years of age, unless growth and nutrition have been assessed carefully. Children under 4 years of age only need 400-500 mL f calcium-fortified, plant-based milk replacements per day to meet their calcium requirements. Larger quantities can reduce appetite, nutritional intake and growth.(6)
TABLE 1.5 Specialised formula and indications in cow's milk allergy(6)
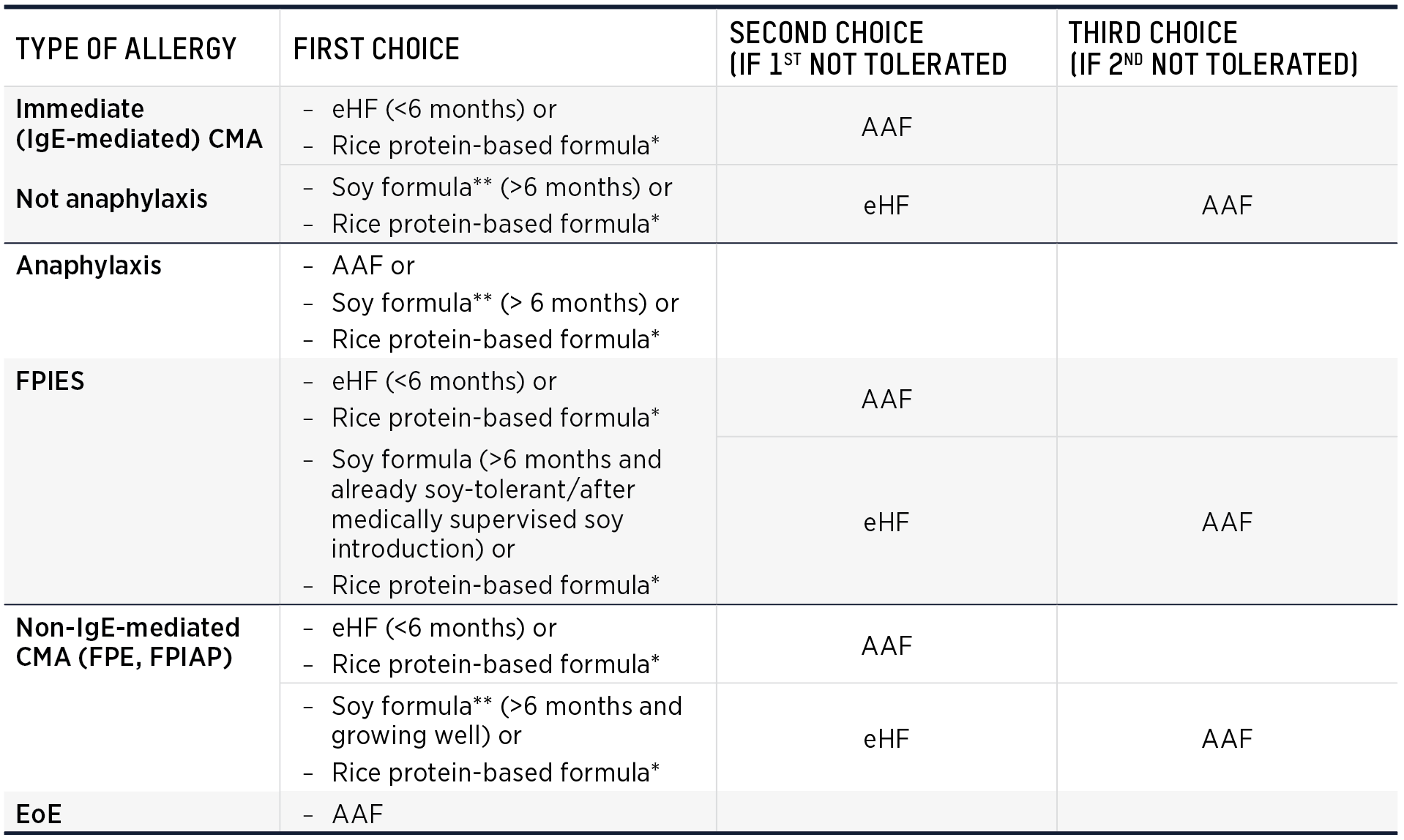 |
Atopic dermatitis (eczema) alone is not an indication for specialised infant formula.
*Unless allergic to rice **Unless allergic to soy
NB Soy is offered as an option for IgE-mediated CMA and anaphylaxis based on expert opinion and review of the literature. The literature presents very limited evidence of IgE-mediated clinical reactions to soy in children with IgE-mediated CMA.
Suitable cow’s milk alternatives in toddlers and older children
It is essential that cow's milk, yoghurt and cheese alternatives with adequate calcium, fat, protein and energy be offered after the child reaches 2 years of age to ensure optimal growth and development. Many plant-based milks are not fortified with calcium and have inadequate energy, protein and fat. Suitable alternative milks have at least the following energy, protein, fat and calcium content:
|
|
TABLE 1.6 Calcium requirements(7)
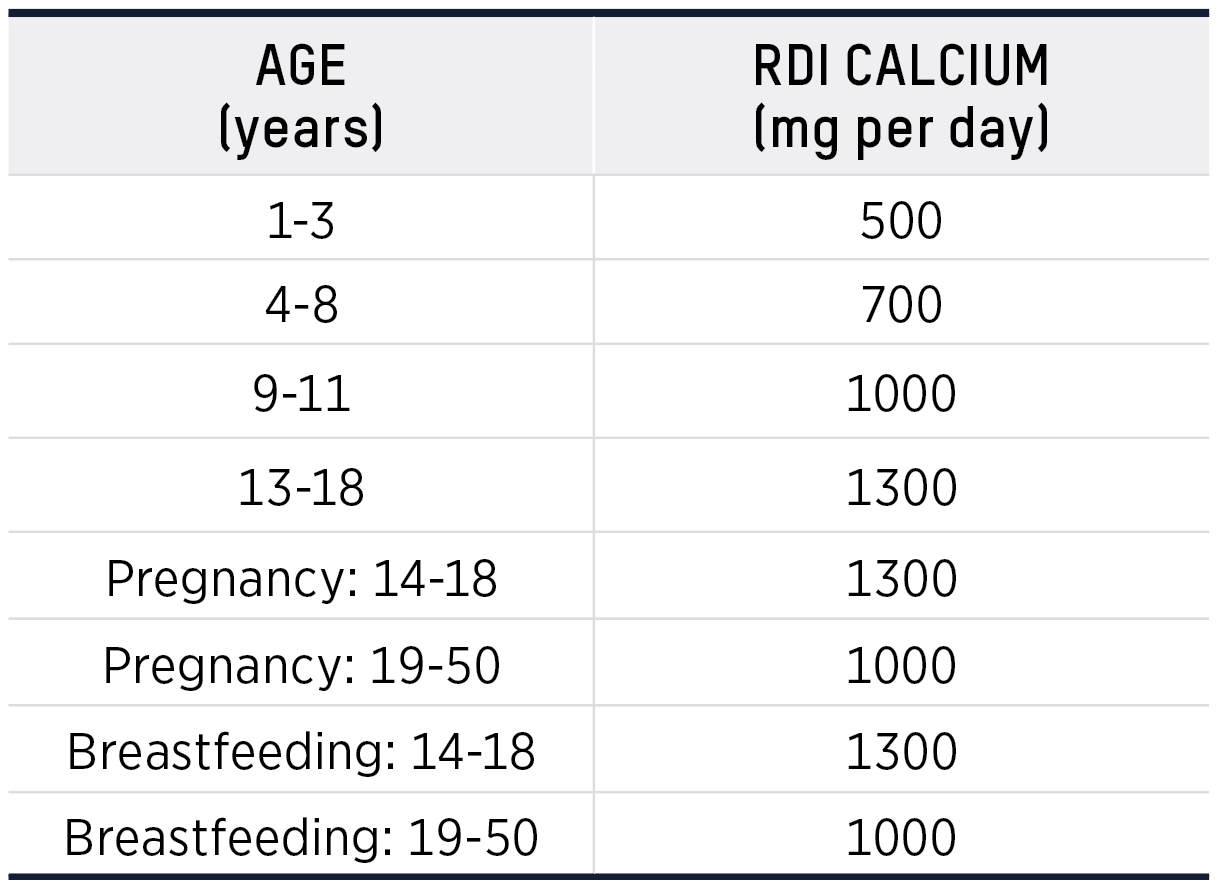 |
It is also important to introduce a cow’s milk alternative yoghurt during the first few years of life to introduce a “creamy texture” so that dairy products are accepted when the cow’s milk allergy
is outgrown. Several plant based yoghurts are available with some being fortified with calcium. Calcium fortified plant based cheese and calcium rich tuna are also available.
Management of Non-IgE-mediated cow’s milk allergy
For breastfed infants with suspected non-IgE-mediated cow’s milk allergy, exclusion of cow’s milk from the maternal diet for at least 2 weeks and up to 4 weeks is recommended. It can take up
to 4 weeks for symptoms to resolve. At the end of the exclusion of cow’s milk, a trial reintroduction is recommended to confirm that cow’s milk is causal. This trial is important to avoid unnecessary exclusion of cow’s milk. Adequate nutritional substitution is essential in both the maternal and infant diet.
Cow’s milk should be excluded from the maternal and infant diet until the infant reaches 9–12 months, or for at least 6 months after symptom resolution. At this point a planned introduction of cow's milk to the infant, using the iMAP cow's milk ladder and recipes can be undertaken.(8)
EOE -- primarily affects the gastrointestinal tract but differs in presentation and chronicity to purely non-IgE-mediated allergies or enzyme deficiencies such as lactose intolerance. EoE involves eosinophils, a type of white blood cell, infiltrating the esophageal tissue, leading to inflammation and symptoms like swallowing difficulty and food impaction.
References
1. Sicherer, S. H., & Sampson, H. A. (2014). Food allergy: Epidemiology, pathogenesis, diagnosis, and treatment. Journal of Allergy and Clinical Immunology, 133(2), 291-307. DOI: 10.1016/j.jaci.2013.11.020.
2. Caubet, J. C., & Szajewska, H. (2017). Non-IgE-mediated gastrointestinal food allergies in children. Pediatric Allergy and Immunology, 28(1), 6-17. DOI: 10.1111/pai.12682.
3. Nowak-Wegrzyn, A., Chehade, M., Groetch, M. E., et al. (2017). International consensus guidelines for the diagnosis and management of food protein-induced enterocolitis syndrome: Executive summary—Workgroup Report of the Adverse Reactions to Foods Committee, American Academy of Allergy, Asthma & Immunology. Journal of Allergy and Clinical Immunology, 139(4), 1111-1126. DOI: 10.1016/j.jaci.2016.12.966.
4. Leonard, S. A., Nowak-Wegrzyn, A. (2015). Food protein-induced enterocolitis syndrome: An update on natural history and management. Current Opinion in Allergy and Clinical Immunology, 15(4), 346-350. DOI: 10.1097/ACI.0000000000000189.
5. Caubet, J. C., & Nowak-Wegrzyn, A. (2011). Current understanding of the immune mechanisms of FPIES. Expert Review of Clinical Immunology, 7(3), 317-327. DOI: 10.1586/eci.11.16.
6. Guide for Milk Substitutes in Cow’s Milk Allergy [Internet]. [cited 19 February 2023]. Available from: Available from: https://www.allergy.
org.au/images/stories/pospapers/ASCIA_HP_Guide_CMA_Milk_Substitutes_2022.pdf
7. NHMRC. Nutrient Reference Values. [Internet]. [cited 19 March 2023]. Available from: https://www.eatforhealth.gov.au/nutrientreference-
values
8. The GP Infant Feeding Network. The Milk Allergy in Primary Care (MAP) Guideline 2019. [Internet]. [cited 19 March 2023]. Available from:
https://gpifn.org.uk/imap