| HOME HEALTH RECORD OCTOBER-JANUARY |  |
||||||||||
| Lillie Dick | Gender: Female | 72 yrs | DOB: 03/10/YEAR | Pref Lang: English | |||||||||||
 |
Patient # |
Last Name |
First Name |
Bed |
|
MRN |
CSN |
Preferred Language |
Patient Class |
|
|
|
||||
| Attend Provider: D Luickas, MD |
Address | Status | ||
| DOB | ||||
| Home Ph | Age | |||
| Last Note | Work Ph | Sex | ||
| Employer | Marital Status | |||
| D Luickas, MD Oncology Specialist |
H&P Date of Service: MONTH/DAY/YEAR HR:MIN Signed Creation Time: MONTH/DAY/YEAR HR:MIN |
-
+ PATIENT ADMINISTRATION
-
PATIENT CHECKLIST Allergies & ARS NKA Alerts !!! HIGH RISK OF FALLS Waterlow Assessment Overdue Skin Assessment Scheduled DD/MM/YYYY 
Home Care Falls Risk Assessment
1. History of falls unknown (0)
2. Mental Status - N/A (0)
3. Vision - patient wears eyeglasses continually (1)
4. Toileting - with assistance (0)
5. Transfer Score - Unstable - limited sitting balance, mechanical lift (3)
6. Mobility Score - Immobile (3)Score = 7
Immunistation / Infection Contact Vaccine Disease Current Scheduled 1. Hib Influenza Type B ✓ - 2. DTaP Diphtheria, Tetanus and Pertussis ✓ - 3. PPSV23 Pneumococcal polysaccharide ✓ - 4. PCV13 Pneumococcal ✓ - 5. Zoster Zoster recombinant Scheduled 18/10/YYYY 6. Twinrix Hepatitis A and B Scheduled 18/10/YEAR, 16/11/YYYY, 7. COVID -19 Moderna COVID-19 ✓ Booster scheduled 16/MM/YYYY, Home Care Home Care Orders Nursing Care Instructions ✓ Physician Summary Scheduled Home Care Information Discharge Planner (to be assigned) Scheduled Care Criteria Medication regimen
Medication review
Self-care assessment
Home-assist review
Dietitian Review
Hospital transferCompliant
Complete
Complete
Complete
Ongoing
As requiredSubstance Use Risk Screen Abbreviated Mental Health Test * Delirium Risk Assessment Tool PATIENT REQUIREMENTS Please make available at all times. Glasses Prescription glasses, sliver wire frame Dentures (upper, lower, full) N/A Prosthesis (hearing aids, eye, limb) N/A Contact Lenses N/A Devices Iphone, tablet Walker Park beside bed at all times CONTACTS Name/Phone Number DOCTOR (GP) PHONE: 0417 004 654 (After hours: 0418 022 345) DIETITIAN PHONE: 0418 222 798 PHARMACIST PHONE: 0417 222 987 DISTRICT NURSE PHONE: 0418 002 456 NEAREST HOSPITAL PHONE: 07 417 111 650 (Monday to Sunday: 9.00am-5.00 pm) CARERS Evelyn: 0418 032 354 CHAPLAINCY Telephone 0400 032 344 and ask for on-call Chaplain DISTRICT HOSPICE PHONE: 07 900 254 143 (Monday to Friday: 9.00am-5.00 pm)
-
+ MEDICAL/LEGAL FORMS
-
-
+ FORMS
-
- Bank of America
- Superannuation
- Contact son, Bradly Dick
Suncorp (Australia)
-
+ PALLIATIVE CARE SUPPORT PLAN
-
DOCUMENTATION/INFORMATION RECEIVED Date and Time Record Author July
DocumentationCaring for Dying Patient Document
D Luikas, Dietitian, Nurses/Pharmacy, Carer
Palliative Care (Australia)
May-June
DocumentationFebruary-April
DocumentationOctober-January
DocumentationD Luickas, MD 2 yrs & 2 months ago
Referral for PEG placementPhysican's referral for Dietitian
Educational Link (Tube Feeding) provided
Patient Information for Constipation provided
Dietitian's Progress Note
D Luickas, MD
Dr Jones
Dietitian
Dietitian
Dietitian
Dietitian
3 yrs ago
General nutrition consultationOriginal medical referral and nutrition progress note Dietitian -
PALLIATIVE CARE SUPPORT PLAN OCTOBER - JANUARY Eligibility Service Approved Frequency Carer Notes Updated Social outings Weekly (Friday) Lillie, while eligible, has opted not to participate in social outings for the past 3 months. Transport Monthly or as requested Transportation to and from oncologist appointments Cleaning Weekly (Tuesday 10:00 am) K Frances (Caretaker and Cleaner) Bathing, hygiene and grooming Two times weekly (Monday 8:00 am / Thursday 8:00 am) M Reily (Nurse) Help with impairments or continence — Not applicable at this stage. Reassess monthly. Meals and food preparation Daily K Frances (Caretaker and Cleaner) / Evelyn (carer) Was tolerating small quantities of soft food. Ceased Oct.
Tolerating 3 cans 2 Cal/mL four days per week
and 2 cans 2 Cal/mL three days per weekNursing Two times weekly (Monday 8:00 am / Thursday 8:00 am) M Reily (Nurse) Including wound care and checking pump feeds. Speech therapy — Not applicable at this stage. Podiatry As required J Carter (Podiatrist) Not applicable at this stage. Occupational therapy or physiotherapy services Two-monthly Dietetic services
Formula
Syringes
Replacement PEG tubesAs required
ABC Pharmacy - ORDER - 80 cans monthly
ABC Pharmacy - ORDER - 160 syringes monthly
ABC Pharmacy - ORDER - 10 sets months
ABC Pharmacy - ORDER - 10 sets monthlyEvelyn (carer) Pharmacy to deliver feed and equipment first Monday of month Pharmaceutical services Monthly G Young (Pharmacist)
-
-
+ FAMILY, SOCIAL, MEDICAL HISTORY
-
PATIENT HISTORY
-
+ PROBLEM LIST
-
HISTORY OF MEDICAL ISSUES Ongoing Problem List Date Opened Status Neutropenia - chemotherapy ceased July Closed Terminal July Ongoing Palliative care - Deteriorating (Phase 3) May (Age 72) Ongoing PEG feeds February (Age 72) Ongoing Palliative care - Unstable (Phase 2) February (Age 72) Ongoing Significantly reduced appetite/feed tolerance February (Age 72) Ongoing Vomiting and esophageal dysmotility October (Age 72) Ongoing Reduced appetite October (Age 72) Ongoing Reduced tolerance for PEG feeds October (Age 70) Ongoing Palliative care - Stable (Phase 1) October (Age 70) Ongoing Neutropenia - chemotherapy halted 2 years ago (Age 70) Ongoing Percutaneous endoscopic gastrostomy (PEG) feeding tube 2 years ago (Age 70) - Outpatient Gastrointestinal Medicine Clinic Ongoing Malnutrition 2 years ago (Age 70) Ongoing Constipation (due to opioid medication) 2 years ago (Age 70) Ongoing Gastro-esophageal reflux disease (GERD) (ICD-10 K 21.9) 2 years ago (Age 70) Ongoing Hypothyroidism (ICD-10 E 039) 2 years ago (Age 70) Ongoing Tachycardia (ICD-10-CM R00.0) 2 years ago (Age 70) Ongoing Cancer treatment - Experimental drug trial and chemotherapy 3-2 years ago (Age 69-70) Closed Breast cancer recurrence - metastasized to bones 3 years ago (Age 69) Ongoing Remission established 16 years ago (Age 56) Closed Breast cancer diagnosis 19 years ago (Age 53) Ongoing Esophageal dysmotility 32 years ago (Age 40) Ongoing
-
Date and Time Type of Encounter Author July Dietetic Consultation
Nutrition Review - Doctor's referral for review
PEG Intake
- Lillie has asked that PEG feeds be provided on request only. Patient reports concern that she will lose capacity without ongoing enteral feeding
- Patient trialed 1 x 250 mL cans 2 cal/mL enteral feed provided by carer yesterday, resulting in nausea, vomiting and explosive diarrhea 30 minutes after feed
- Ongoing constipation prior to prevent PEG feed trial. Small motion 1-2/7
- Tolerating fourth hourly 40 mL water flushes to provide 240 mL water/24 hours
- Patient continues to experience abdominal pain and nausea today
- Nil appetite
Oral Diet
- 200 mL water daily as sips provided by carer
- No longer tolerating oral diet
- Medications provided via PEG tube
Plan
- Dietitian to prepare plan in Activity 16.4.4
- Please leave gastrostomy tube insitu in the event of Lillie passing
May-June Dietetic Consultation
PEG Feed Review - Doctor's referrral for PEG feed review
PEG Intake
- Currently tolerating 1 x 250 mL cans 2 cal/mL enteral feed daily
- Tolerating fourth hourly 60 mL water flushes to provide 360 mL water/24 hours
Oral Diet
- Managing oral intake independently
- 600 mL water daily as sips
- Lillie managing a few teaspoons of apple sauce, milk pudding and cooked oatmeal daily.
Plan
- Dietitian to prepare plan in Activity 16.3.4
- Sit patient in chair or lay with head raised to at least 30 degrees or on three pillows
- Remain elevated after feeding for 30-60 minutes
- If patient starts to cough, cease feed immediately and contact the hospital
- Please continue to record feed and oral fluid intake
February-April Dietetic Consultation
PEG Feed Review - Doctor's referrral for PEG feed review
PEG Intake
- Lillie manages occasional mouthfuls of pureed cooked foods; apple sauce, milk pudding to provide <300 kJ (<75 kcal) daily
- Currently tolerating 1-2 x 250 mL cans 2 cal/mL enteral feed daily
- Tolerating fourth hourly 60 mL water flushes to provide 360 mL water/24 hours
Oral Diet
- 700 mL water daily as sips
- Pureed cooked diet as tolerated; apple sauce, milk pudding
Plan
- Dietitian to prepare plan in Activity 16.2.4
- Sit patient in chair or lay with head raised to at least 30 degrees or on three pillows
- Remain elevated after feeding for 30-60 minutes
- If patient starts to cough, cease feed immediately and contact the hospital
- Please continue to record feed and oral fluid intake
Dietitian January Dietetic Consultation
PEG Feed Review - Patient's/carer's request for PEG feed review
PEG Intake
- Feed pump tubes disconnecting from pump during night feed
- Currently tolerating 3 x 250 mL cans 2 cal/mL enteral feed four days/wk and 2 x 250 mL cans 2 cal/mL enteral feed three days/wk
Aiming for 3 x 250 mL cans 2 cal/mL enteral feed daily - Tolerating fourth hourly 60 mL water flushes to provide 360 mL water/24 hours
Oral Diet
- Tolerating 700 mL water daily as sips
- Tolerating several tablespoons of pureed cooked diet daily; apple sauce, milk pudding
- Intake record below.
Plan
- Dietitian to prepare plan in Activity 16.1.5
- Sit patient in chair or lay with head raised to at least 30 degrees or on three pillows
- Remain elevated after feeding for 30-60 minutes
- If patient starts to cough, cease feed immediately and contact the hospital
- Please continue to record feed and oral fluid intake
- Assess PEG site every shift for signs of leakage, inflammation, infection or pain at the stoma site
- Clean PEG site daily according to site based guidelines. Allow to dry thoroughly and leave exposed.
Dietitian October Medical Assessment
- Patient neutropenic (Absolute Neutrophil Count <0.5 x 109 cells/L)
- Nil sign of infection/fever
- Cease chemotherapy with a view to reinstating recovery of ANC
- Repeat bloods 1/52
- Optimise oral and skin hygiene
- Strict hand-washing protocols before and after patient contact
- Strict hygiene protocol with PEG feed provision
- Monitor for associated complications; thrombosis, cytopenias, constipation
- Monitor for signs of infection
Dr Jones (GP) October PEG Feed Review - Doctor's referrral for PEG feed review
PEG Intake
- Currently tolerating 3 x 250 mL cans 2 cal/mL enteral feed four days/wk and 2 x 250 mL cans 2 cal/mL enteral feed three days/wk
- Tolerating fourth hourly 60 mL water flushes to provide 360 mL water/24 hours. Use of syringe in side tap of feeding tube.
- Patient has requested PEG feed to be provided at a tolerated rate.
She is aiming for 3 x 250 mL cans 2 cal/mL enteral feed daily
See schedule in Diet Orders below - Please continue to record feed and fluid intake
- Patient unsteady on feet. Cease home weighing
Oral Intake
- Patient tolerating a small quantity of soft diet. Vomiting, nausea and esophageal dysmotility ongoing when intake exceeds 1/2 cup in any one meal
- Reduced appetite/desire to eat
- Tolerating 700 mL water daily as sips
- Intake record below.
Plan
- Dietitian to prepare plan in Activity 16.1.4
- Sit patient in chair or lay with head raised to at least 30 degrees or on three pillows
- Remain elevated after feeding for 30-60 minutes
- If patient starts to cough, cease feed immediately and contact the hospital
- Please continue to record feed and oral fluid intake
6 months prior Dietetic Consultation
- Patient consuming 1 -2 cans of 2 kcal tube feed using feeding pump
- Not tolerating oral diet
- Soft pureed diet as per patient request. Patient consuming < 100 kcal/day orally.
Dietitian 18 months prior Dietetic Consultation
- Tolerating 3 cans of 2 kcal PEG feed using feeding pump
- Managing a small amount of soft foods daily to provide 300 cal, 1 200 kJ
- Patient reports she lacks energy and is disinterested in foods
- Continue with PEG feeds as tolerated
- Soft pureed diet as per patient request
Dietitian 2 years ago Dietetic Consultation (HENT Third Visit)
- Introduction of soft oral foods/fluids as tolerated
(~300 kcal/can) of 2.0 kcal/mL overnight feeding via feeding pump
Dietitian 2 years ago Dietetic Consultation (HENT Second Visit)
- Night feeding recommended for 2 000 kcal (4 cans) with 2 kcal/mL feed using feeding pump
Dietitian 2 years ago Emergency Room for Constipation
- Senna medication subscribed
ED Doctor 2 years ago Dietetic Consultation (Phone Call)
- Lillie not tolerating bolus feeding. Changed to gravity feeding equipment supplies
Dietitian 2 years ago Dietetic Consultation (Phone Call)
- Patient experienced gastric symptoms when feeds were "sped up"
- Changed feed to 4 cartons of 2.0 kcal/mL per day
Dietitian 2 years ago Dietetic Consultation (HENT First Visit)
- Initiation of bolus feeding with 5 cartons of 1.5 kcal/mL per day
Dietitian 2 years ago PEG Insertion - Insertion of percutaneous endoscopic gastrostomy (PEG) feeding tube by gastroenterologist for malnutrition
Dr Jones (GP) 2 years ago Cancer Treatment
- The experimental drug trial is discontinued
- Chemotherapy, Ibrance commences. See Lillie's Medications
Dr Luickas (Oncologist) 3 years ago Breast Cancer Recurrence
- Commencement of 6 weekly oncologist appointments
- Commencement of experimental drug trial
- General nutrition consultation
Dr Luickas (Oncologist)
-
+ PROGRESS NOTES
-
Date and Time Note Type Author 6 months ago Nutrition Progress Note 2 Years Ago (Age 70) Nutrition Progress Note (Home enteral nutrition/Third Visit) 2 Years Ago (Age 70) Nutrition Progress Note (Home enteral nutrition/Second Visit) 2 Years Ago (Age 70) Nutrition Progress Note (HENT First Visit) Dietitian 2 Years Ago (Age 70) Nutrition Quality of Life 36-Item Short Form Survey (HENT First Visit) Dietitian and Patient 2 Years Ago (Age 70) Physician Consultation Request - For dietitian's instruction on bolus feed Dr Luickas (Oncologist) 3 Years Ago (Age 69) Initial Physician Referral and Nutrition Progress Note Dr Luickas (Oncologist) & J Hart (Oncology Dietitian)
-
+ TEST RESULTS AND PROCEDURES
-
+ Biopsy – Breast Screening Date and Time Mammogram & Ultrasound Author 2 Years Ago 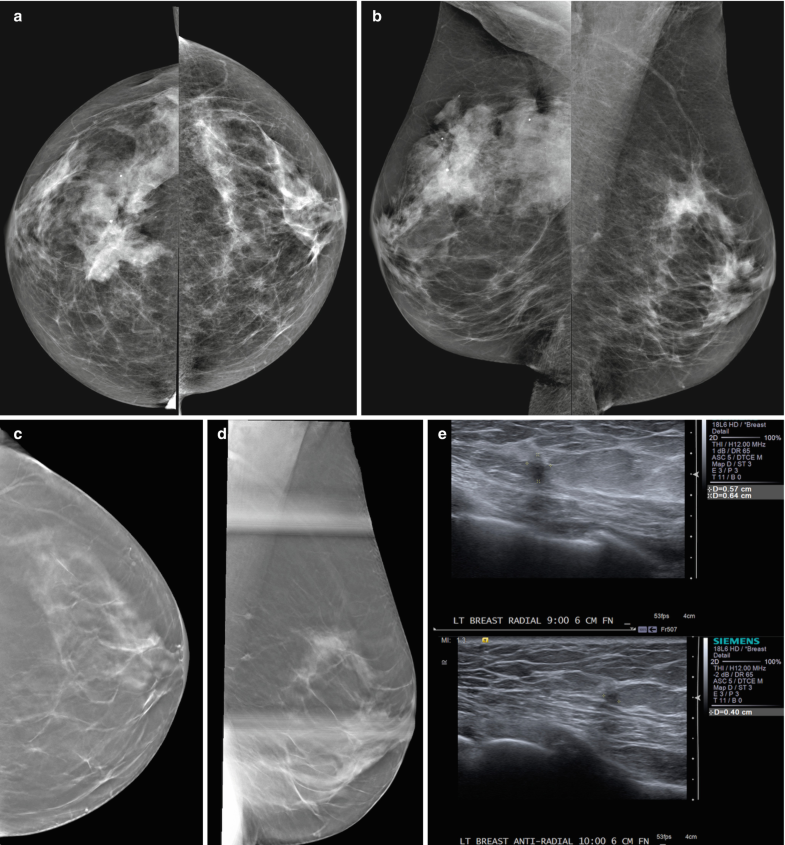
Dr D Luickas Notes:
Screen-detected multifocal invasive ductal carcinoma III between the 9 and 10:00 axis of the left breast in a 70-year-old patient with a personal history of right breast cancer, breast conserving therapy and radiation treatment at age 53.
(a, b) CC and MLO views: Post-surgical changes are present in the right breast. There are two new irregular shaped and partially spiculated masses in the 9 and 10:00 axis of the left breast posterior depth which are best appreciated on additional tomosynthesis views CC
(c) and ML
(d, spot). On targeted ultrasound
(e) these correspond to two irregular shaped and marginated hypoechoic masses (9:00 6 cm from the nipple 0.6 × 0.5 cm, 10:00 6 cm from the nipple 0.4 × 0.4 cm)
Reference:
Gilbert FJ, Pinker-Domenig K (2019) Diagnosis and Staging of Breast Cancer: When and How to Use Mammography, Tomosynthesis, Ultrasound, Contrast-Enhanced Mammography, and Magnetic Resonance Imaging. In: Hodler J, Kubik-Huch R, von Schulthess G (eds) Diseases of the Chest, Breast, Heart and Vessels 2019-2022. IDKD Springer Series. Springer, Cham. https://doi.org/10.1007/978-3-030-11149-6_13+ Bone Scintigraphy + CT Scan
-
+ BLOOD TESTS
-
Biochemical Data and Medical Tests and Procedures
Test 3 Years Ago 2 Years Ago October-January Comments Electrolyte and
Renal ProfileUrea M>50 (3.0-8.5 mmol/L) F>50 (2.5-7.5 mmol/L) 4.8 4.6 3.2 Calcium (2.1-2.60 mg/dL) 2.5 2.2 2.4 Creatinine (0.8-1.3 mg/dL) 0.9 1.2 1.1 Sodium (135-145 mmol/L) 140 141 139 Potassium (3.5-5.0 mEq/L) 4.0 4.2 4.9 White Cell Profile WBC (4.8-11.8 billion cells/L) 1 x 109 1.5 x 109 0.98 x 109 The typical lower limit of the neutrophil count is about 1500 cells per microliter of blood (1.5 × 10 9 cells per liter). As the count goes below this level, the risk of infection increases. Neutropenia severity is classified as: - Mild: 1 000 to 1 500/mcL (1 to 1.5 × 109/L)
- Moderate: 500 to 1 000/mcL (0.5 to 1 × 109/L)
- Severe: below 500/mcL (0.5 × 109/L)
Cardiac Biomarkers/EnzymesTroponin T (0.0-0.10 µg/mL) 0.09 0.09 0.1 Creatine Kinase (CK)
- - - BNP or NT-proBNP (10-35 U/L) - - - Prolonged prothrombin time (12 sec) - - - Bilirubin (> 1.5 mg/dL) 1.6 1.8 - Glucose/
Endocrine Profile
Glucose, random
(3.0-7.7 mmol/L)6.7 4.2 3.8 HbA1c (<6%/<42 mmol/mol) 5.8 4 3.2 Inflammatory Profile C-reactive protein (undetected) (< 3 mg/L) 2.7 3.1 -
Nutritional Anemia ProfileHemoglobin (12-15 mg/dL) 13 12 - Hematocrit (37-47%) 40 41 - Myoglobin (30-90 µg/mL) 58 67 - Protein Profile Albumin (3.5-5.0 g/dL) 3.3 3.2 3.3 Lipid Profile
Triglycerides (35-135 mg/dL) 40 39 - Cholesterol (< 5.2 mmol/L) 5.5 5.1 - HDL Cholesterol (1.0 - 2.5 mmol/L) 1.4 1.3 - LDL Cholesterol (< 3.5 mmol/L) 3.7 3.3 -
-
+ VITALS AND WEIGHT
-
Item Name 3 Years Ago 2 Years Ago OCTOBER - JANUARY Comments Pulse 70 72 60 88 84 66 80 75 56 O2 Sat In range In range In range Temp Normal Normal Normal Nil fever Enteral Feed Intake Order (mL) 1 Litre 2 Cal Enteral Formula 750 mL 2 Cal Enteral Formula Tolerating 750 mL 4 days/week and 500 mL 3 days/week Oral Fluid Intake (mL) 500 mL Urine Output (Ave. mL) 1 800 mL 1 700 mL 1 500 mL IV Fluid Intake (Ave. mL) NIL Dietary Intake: Breakfast & Morning Snack 1/4 cup cooked oatmeal/1/4 cup canned apple sauce 1/4 cup cooked oatmeal; 1/4 cup canned apple sauce 1/4 cup canned apple sauce Dietary Intake: Midday Meal & Afternoon Snack 1/4 cup macaroni cheese/1/4 cup canned pudding 1/4 cup macaroni cheese/1/4 cup canned pudding 1/4 cup canned pudding Dietary Intake: Evening Meal and Evening Snack 1/4 cup creamy potato salad 1/4 cup creamy potato salad 1/4 cup macaroni cheese Wt (kg [lb]) SEE WEIGHT CHART BELOW Ht (cm [ft]) 155 (5'1") BMI (kg/m2) 32.77 kg/m2 27.5 kg/m2 27.5 kg/m2 Cease patient weighs Pain Level (0 to 5)
0=no pain; 5=severe pain3 4 4 Maintain paid meds to prevent break-through pain Date PEG Tubes Changed DATE Date tube put in: X/XX/XXXX X/XX/XXXX X/XX/XXXX X/XX/XXXX Date changed Gauge size on tube Number on tube RESPIRATORY RATE DATE am pm WEIGHT HISTORY .png)
DATE 25 Years Ago
(Age 45)8 Years Ago
(Age 64)3 Years Ago
(Age 69)2 Years Ago
(Age 70)4 Months Ago (June)
(Age 71)3 Months Ago (July)
(Age 71)2 Months Ago (August)
(Age 71)October
(Age 71.5)Measured Weight 83.9 kg (185 lb) 78.5 kg (173 lb) 78.5 kg (173 lb) 78.5 kg (173 lb) 66 kg (146 lb) 66.7 kg (145 lb) 68.6 kg (151 lb) 66 kg (146 lb) BMI 34.9 kg/m2 32.77 kg/m2 32.77 kg/m2 32.77 kg/m2 27.5 kg/m2 27.7 kg/m2 28.7 kg/m2 27.5 kg/m2 Author Dr Jones Dr Jones Dr Jones Dr Jones Dr Jones & Dietitian
12.5 kg (27 lb) weight loss in past month (Dietitian's Visit 1 for HENT)
Dr Jones & Dietitian
2 weeks following PEG Insertion
(Dietitian's Visit 2 for HENT)Dr Jones & Dietitian
8 weeks following PEG Insertion
(Dietitian's Visit 3 for HENT)Dr Jones
CEASE HOME WEIGHING
-
+ ORDERS/OBSERVATIONS
-
PALLIATIVE CARE CLINICAL ASSESSMENT TOOLS Date Tool Score Author 1 week ago Australian-modified Karnofsky Performance Status 30 Dr Jones 2 months ago Australian-modified Karnofsky Performance Status 40 Dr Jones 6 months ago Australian-modified Karnofsky Performance Status 50 Dr Jones 2 years ago Australian-modified Karnofsky Performance Status 60 Dr Jones 3 years ago Australian-modified Karnofsky Performance Status 70 Dr Jones
SCAN ORDERS Referral Order COMMENTS MRI Nil X-RAY Nil DOPPLER Nil
OBSERVATIONS Nurse/caregiver Simple Oxygen Not required Vital Signs Times: as needed, until specified per nursing routine Strict Input and Output Routine: every 4 hrs, first occurrence day 1, until specified Activity Level Routine: continuous starting as needed day 1, until specified
As toleratedNotify Physician If... Notify physician pulse < 50 bpm, or > 100 bpm, notify physician for SBP < 90/ Weight Frequency Prior October - Monthly/Cease October forward Other Sequential compression devices while in bed
Move patient hourlyPain Assessment Routine: every 4 hrs, first occurrence day 1, until specified Comfort Level Assessment Routine: every 4 hrs, first occurrence day 1, until specified FLUID ORDERS DIETITIAN SYRINGE WATER FLUSHES (BEFORE AND AFTER FEEDS) Amount (mL) Comments Duration From To Syringe Date Time Date Time 1 10 pm 60 Use of syringe in side tap of feeding tube. 10 mins 10/01/YEAR 1800 hrs 10/01/YEAR 1810 hrs New 2 1 am 60 10 mins 10/01/YEAR 0100 hrs 10/01/YEAR 0110 hrs 3 4 am 60 10 mins 10/01/YEAR 0400 hrs 10/01/YEAR 0410 hrs 4 7 am 60 10 mins 10/01/YEAR 0700 hrs 10/01/YEAR 0710 hrs 5 11 am 60 10 mins 10/01/YEAR 1100 hrs 10/01/YEAR 1110 hrs 6 3 pm 60 10 mins 10/01/YEAR 1500 hrs 10/01/YEAR 1510 hrs TOTAL 240 mLs TOTAL 60 MINS/24 hrs
-
+ MEDICATIONS
-
MEDICATION ORDERS, HOME Name Dose Route Start Duration Nature Throid 65mg 1 Oral — Do Not Crush Morning (1) Amitiza 25 mcg1 2 Oral — Do Not Crush Morning (1) and Bedtime (1) Ducosate Sodium 100 mg 3 Oral — Do Not Crush Morning (1) and Bedtime (2) Ibrance 100 mg 1 Oral — Do Not Crush CEASE Duloxetine (Cymbalta) 60 mg 1 Oral — Open capsule and mix with applesauce/yoghurt Morning (1) Omeprazole (Prilosec) 20 mg 1 Oral — Open capsule and mix with applesauce/yoghurt Morning (1) Multi-vitamin/mineral supplement 1 Oral — Crush and mix with applesauce/yoghurt Morning (1) Psyllium 3 Oral — Open capsule and mix with applesauce/yoghurt Morning (2) and Bedtime (1) Prednizone 10 mg 0.5 every other day Oral — Crush and mix with applesauce/yoghurt Morning (0.5 every other day) Buproprion (Wellbutrin) 75 mg 1 Oral — Crush and mix with applesauce/yoghurt Morning (1) Culturelle 1 Oral — Open capsule and mix with applesauce/yoghurt Morning (1) Metaclopramide liquid (Reglan) 5 mg/5 mL 10 mL Oral — Before feedings and meals Morning (5 mL) and Bedtime (5 mL) Ondansetron (Zofran) 4 mg As required Dissolve on tongue as needed for nausea every 8 hours Morphine oral 20 mg/ml as needed for pain 0.5-1.0 every 4 to 6 hours As required Oral Bedtime (0.5 mL) Senna laxative 20 mL Tube Morning (10 mL) and Bedtime (10 mL) Dulcolax suppository As required Insert as directed on package Duragesic patch (Fentanyl) 25 mcg/hr Change every 72 hours Lidocaine patch As required Cut in half and apply to ribcage where pain is located every night or as needed Bedtime
-
+ DIET
-
DIET/NUTRITION ORDERS Diet Order Date Started Date Discontinued PEG Feeding Regimen
Goal 3 x 250 mL can of 2 kcal enteral feed per 24 hours
60 mL water flushes before and after feeds
Fourth hourly 60 mL water flushes 7am to 10 pm
Oral intake as desired
OCTOBER
ENTERAL FEEDING PLAN - Fiber-Free 2 Cal/mL Formula METHOD SITE PERIOD Continuous Tube Feeding (Pump) PEG DURATION
(hrs/min)FROM TO RATE
(ml/hr)FLUID TYPE AMOUNT (mL) Date Time Date Time 1 Water (flush) 60 mL 10 mins OCT - JAN 10 pm OCT - JAN 2 Enteral Formula (2 kcal) 250 mL 3 hrs 10 pm 10 am 85 mL 3 Water (flush) 60 mL — 1 am 4 Enteral Formula (2 kcal) 250 mL 3 hrs 1 am 12 pm 85 mL 5 Water (flush) 60 mL — 4 am 6 Enteral Formula (2 kcal) 250 mL 3 hrs 4 am 2 pm 85 mL 7 Water (flush) 60 mL — 7 am TOTAL 990 mL 9 hrs THERAPEUTIC DIET DIET DIET Normal diet Gluten-free Nil by mouth (NBM) Lactose-free Fluid restriction (specify): ________________________________ L/day Low-lactose Clear fluids Low-amine Diabetic clear fluids Low FODMAPS Free fluids Low microbial diet Thickened fluid (specify): ________________________________ Texture modified food (specify): __soft, pureed______ No added salt (NAS) Low fibre/low residue Low protein High fibre Low potassium High energy/high protein diet Low protein, sodium, potassium Low energy Cardioprotective diet Very low energy Diabetic: Set CHO Vegan Diabetic: Modified CHO Lacto-ovo vegetarian Allergy (specify): ________________________________ Halal Food intolerance (specify): ________________________________ Kosher DIET SUGGESTIONS FROM DIETITIAN ABBREVIATION FOOD BF MT L AT D S Water W Water SW/MW Soda water/Mineral water Milk Drinks M Whole milk SyM Soy milk CM Caramel milk ChocM Chocolate milk ICoM Iced coffee milk SM Strawberry milk VM Vanilla milk Mo Milo FSmth Fruit smoothie Modified Milk Drinks MP Whole milk + polycose* HPM High-protein milk Sodas/Soft Drinks GAle Ginger ale Lmnd Lemonade LC Lemon cordial LimeC Lime cordial OC Orange cordial Juices AJ Apple juice OJ Orange juice PJ Pear juice PrJ Prune juice TJ Tomato juice Fruit and Sweets IC Ice cream Cus Custard J Jelly/Jello Pureed pr Pureed prunes Yoghurts Y Yoghurt, flavoured FY Portion frozen yoghurt, (AFC) Cookies and Crackers SW Sweet wafers (dunk in liquid) SPC Sweet plain cookies (dunk in liquid) Supplement Drinks Bov Bovril CFS Clear fluid soup (Consommé) FS Fortified soup Ens (V/C) Ensure (AFC) Ens + Ensure Plus (Vanilla) Res (O/B) Resource (Orange/Berry) SusW Sustagen + water (AFC) SusSKM Sustagen + skim milk (AFC) SusM Sustagen + whole milk (AFC) * Polycose or Polyjoule ** Cordial also known as squash AFC = Add the flavour code for the product
BF Breakfast MT Morning Tea/Morning Snack L Lunch/Midday Meal AT Afternoon Tea/Afternoon Snack D Dinner S Supper/Evening Snack FOOD / FLUID CONSUMPTION CHARTS Charts Completed By: Assessed By: February-April - Food/Fluid Consumption Chart Nurse Dietitian October-January - Food/Fluid Consumption Chart Nurse Dietitian MALNUTRITION SCREENING TOOL 1. Has the patient lost weight recently without trying?
If yes, how much (kg)?2. Is patient eating poorly or lack of appetite. Total Nutrition Score No (0)
Unsure if has lost weight (2)
Yes: 0.5 – 5 kgs (1)
Yes: > 5 – 10 kgs (2)
Yes: > 10 – 15 kgs (3)
Yes: > 15 kgs (4)
Yes but unsure how much (2)
Yes (1)
No (0)
0 Weight Loss Score: 0 Appetite Score: 0
