Practice Consideration
Cow’s milk is a very good source of high-quality protein, fat, easily assimilated calcium and riboflavin and it has significant levels of vitamin B12, vitamin A, vitamin D, magnesium and phosphate. Cow’s milk exclusion diets can have detrimental effects on growth and development if milk is not adequately substituted. Dietary education must include other names for cow's milk which may be listed under ingredients on the packaging of processed foods.
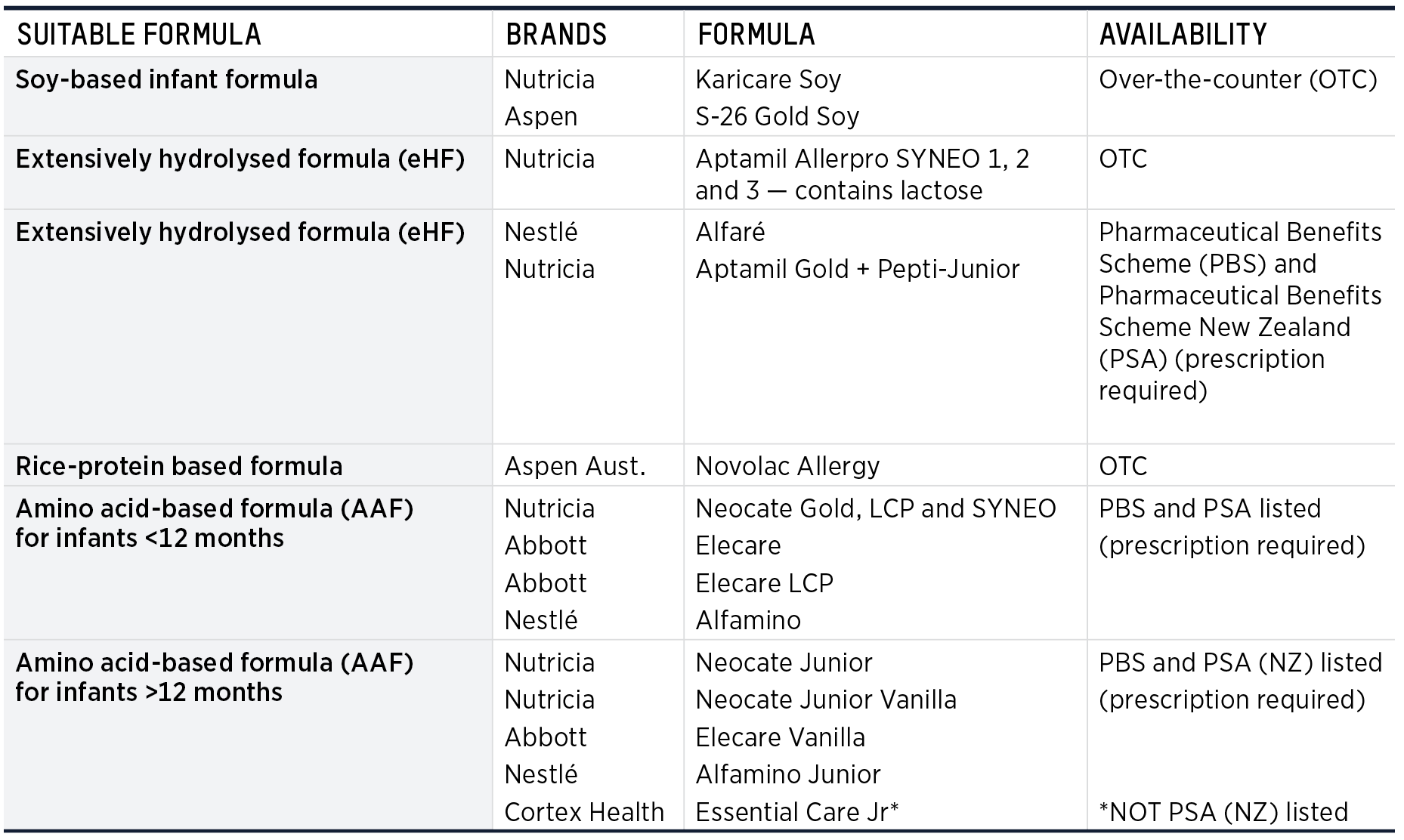
Suitable specialised infant formula for cow's milk allergy
Table 1.4 describes specialised infant formula suitable for cow's milk allergy and indicates which
are appropriate in infants and children who need to avoid cow’s milk protein.(19) Further information is available on www.allergy.org.au
TABLE 1.4 Specialised infant formula suitable for cow's milk allergy (CMA)(19)
 |
Infant Formula NOT Recommended for CMA
The following types of formula are NOT recommended for infants with CMA:
- Standard infant formula including anti-regurgitation, lactose-free, organic, newborn, and follow-on
- Goat milk-based infant formula
- Other mammal milks and formula
- A2 formula
NB For children with cow’s milk and soy allergies, most plant-based milk replacement products that are not fortified with calcium are too low in protein, fat, and calcium. They are not nutritionally adequate for children <2 years of age, unless growth and nutrition have been assessed carefully. Children under 4 years of age only need 400-500 mL
of calcium-fortified, plant-based milk replacements per day to meet their calcium requirements. Larger quantities can reduce appetite, nutritional intake and growth.(19)
TABLE 1.5 Specialised formula and indications in cow's milk allergy(19)
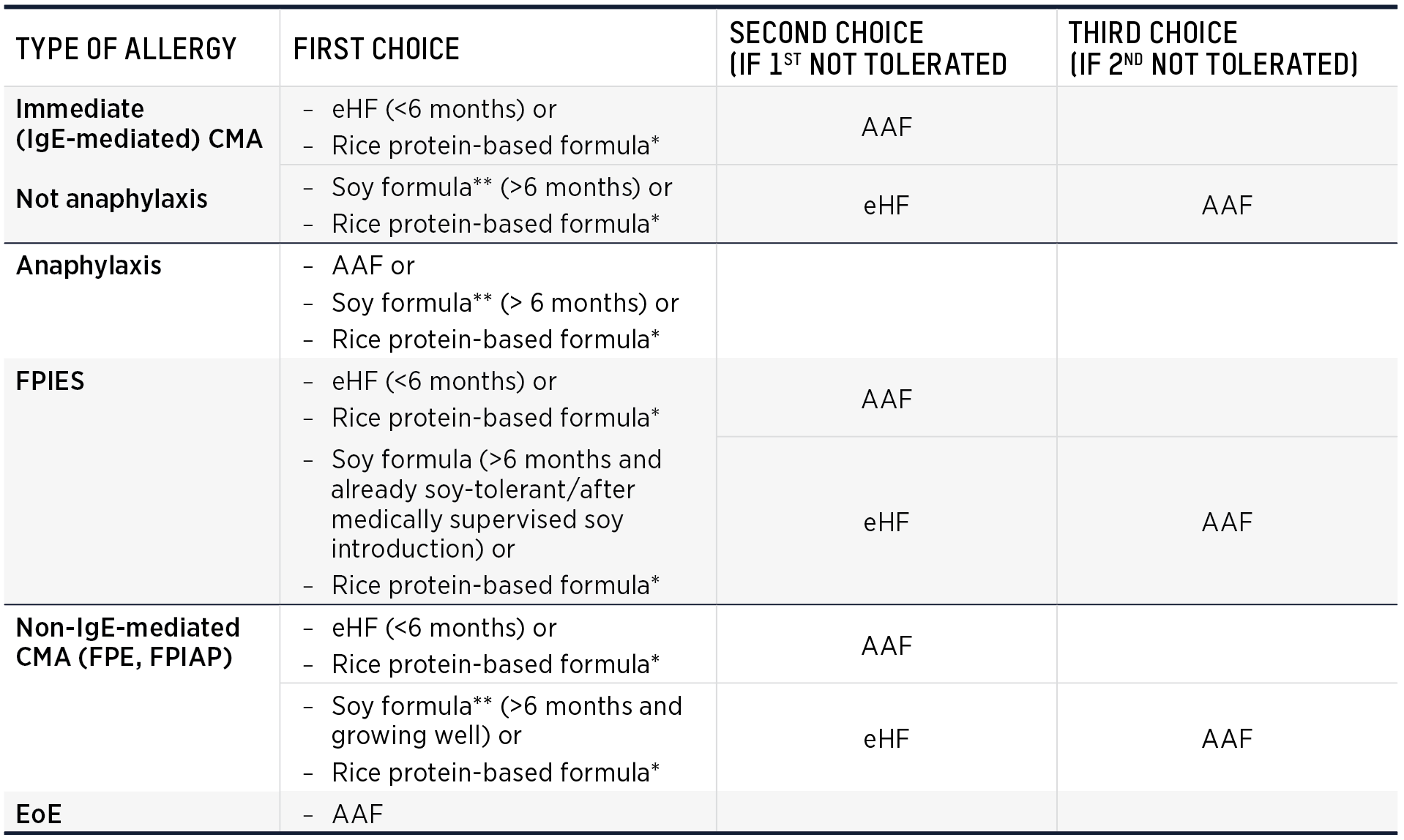 |
Atopic dermatitis (eczema) alone is not an indication for specialised infant formula.
*Unless allergic to rice **Unless allergic to soy
NB Soy is offered as an option for IgE-mediated CMA and anaphylaxis based on expert opinion and review of the literature. The literature presents very limited evidence of IgE-mediated clinical reactions to soy in children with IgE-mediated CMA.
Suitable cow’s milk alternatives in toddlers and older children
It is essential that cow's milk, yoghurt and cheese alternatives with adequate calcium, fat, protein and energy be offered after the child reaches 2 years of age to ensure optimal growth and development. Many plant-based milks are not fortified with calcium and have inadequate energy, protein and fat. Suitable alternative milks have at least the following energy, protein, fat and calcium content:
|
|
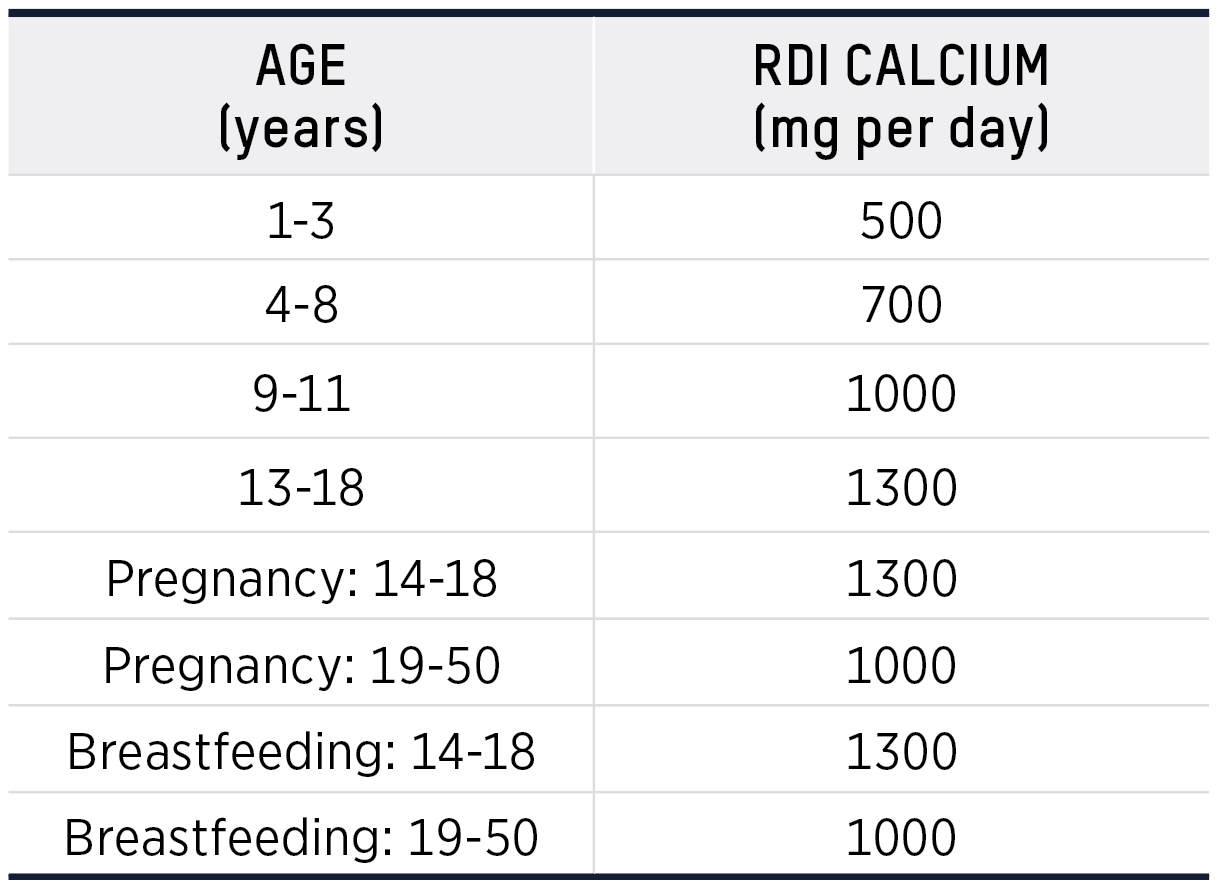
TABLE 1.6 Calcium requirements(20)
 |
It is also important to introduce a cow’s milk alternative yoghurt during the first few years of life to introduce a “creamy texture”
so that dairy products are accepted when the cow’s milk allergy
is outgrown. Several plant based yoghurts are available with some being fortified with calcium.
Calcium fortified plant based cheese and calcium rich tuna are
also available.
Management of Non-IgE-mediated cow’s milk allergy
For breastfed infants with suspected non-IgE-mediated cow’s
milk allergy, exclusion of cow’s milk from the maternal diet for at least 2 weeks and up to 4 weeks is recommended. It can take up
to 4 weeks for symptoms to resolve. At the end of the exclusion
of cow’s milk, a trial reintroduction is recommended to confirm that cow’s milk is causal. This trial is important to avoid unnecessary exclusion of cow’s milk. Adequate nutritional substitution is essential in both the maternal and infant diet.
Cow’s milk should be excluded from the maternal and infant diet until the infant reaches 9–12 months, or for at least 6 months after symptom resolution. At this point a planned introduction of cow's milk to the infant, using the iMAP cow's milk ladder and recipes can be undertaken.(21)
EOE -- primarily affects the gastrointestinal tract but differs in presentation and chronicity to purely non-IgE-mediated allergies or enzyme deficiencies such as lactose intolerance. EoE involves eosinophils, a type of white blood cell, infiltrating the esophageal tissue, leading to inflammation and symptoms like swallowing difficulty and food impaction.
References — Food Allergy and Cow's Milk Protein Allergy
Section 5 provides information and nutrition recommendations on:
|
|
- NIAID-Sponsored Expert Panel, Boyce JA, Assa'ad A, Burks AW, et al. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010 Dec;126(6 Suppl):S1-58.
- Peters R, Koplin J, Gurrin L, et al. HealthNuts Study. The prevalence of food allergy and other allergic diseases in early childhood in a population-based study: HealthNuts age 4-year follow-up. J Allergy Clin Immunol. 2017 Jul;140(1):145-153.e8.
- Sasaki M, Koplin JJ, Dharmage SC, et al. Prevalence of clinic-defined food allergy in early adolescence: The SchoolNuts study. J Allergy Clin Immunol. 2018;141(1):391-8.e4.
- Sicherer SH, Sampson HA. Food allergy: A review and update on epidemiology, pathogenesis, diagnosis, prevention, and management. J Allergy Clin Immunol. 2018 Jan;141(1):41-58.
- Netting MJ, Campbell DE, Koplin JJ, Beck KM, et al. Centre for Food and Allergy Research, the Australasian Society of Clinical Immunology and Allergy, the National Allergy Strategy, and the Australian Infant Feeding Summit Consensus Group. An Australian Consensus on Infant Feeding Guidelines to Prevent Food Allergy: Outcomes From the Australian Infant Feeding Summit. J Allergy Clin Immunol Pract. 2017 Nov-Dec;5(6):1617-1624.
- Sathe SK, Liu C, Zaffran VD. Food Allergy. Annu Rev Food Sci Technol. 2016;7(1):191-220.
- Sicherer SH. Clinical implications of cross-reactive food allergens. J Allergy Clin Immunol. 2001 Dec;108(6):881-90.
- Mullins RJ, Dear KB, Tang ML. Time trends in Australian hospital anaphylaxis admissions in 1998-1999 to 2011-2012. J Allergy Clin Immunol. 2015 Aug;136(2):367-75.
- Caubet JC, Szajewska H, Shamir R, Nowak-Węgrzyn A. Non-IgE-mediated gastrointestinal food allergies in children. Pediatr Allergy Immunol. 2017 Feb;28(1):6-17.
- Nowak-Węgrzyn A, Chehade M, Groetch ME, et al. International consensus guidelines for the diagnosis and management of food protein-induced enterocolitis syndrome: Executive summary-Workgroup Report of the Adverse Reactions to Foods Committee, American Academy of Allergy, Asthma & Immunology. J Allergy Clin Immunol. 2017 Apr;139(4):1111-1126.e4
- Agyemang A, Nowak-Wegrzyn A. Food Protein-Induced Enterocolitis Syndrome: a Comprehensive Review. Clin Rev Allergy Immunol. 2019;57(2):261-71.
- Groetch M, Baker MG, Durban R, et al. The practical dietary management of food protein-induced enterocolitis syndrome. Ann Allergy Asthma Immunol. 2021 Jul;127(1):28-35.
- Caubet JC, Cianferoni A, Groetch M, Nowak-Wegrzyn A. Food protein-induced enterocolitis syndrome. Clin Exp Allergy. 2019 Sep;49(9):1178-1190.
- Academy of Nutrition and Dietetics. Nutrition Terminology Reference Manual (eNCPT): Dietetics Language for Nutrition Care. NCP Step 1: Nutrition Assessment. 2020. [Internet]. [cited 9 September 2022]. Available from: https://www.ncpro.org/pubs/2020-encpt-en/page-015
- Academy of Nutrition and Dietetics. Nutrition Terminology Reference Manual (eNCPT): Dietetics Language for Nutrition Care. NCP Step 2: Nutrition Diagnosis. 2020. [Internet]. [cited 9 September 2022]. Available from: https://www.ncpro.org/pubs/2020-encpt-en/page-036
- Academy of Nutrition and Dietetics. Nutrition Terminology Reference Manual (eNCPT): Dietetics Language for Nutrition Care. NCP Step 3: Nutrition Intervention. 2020. [Internet]. [cited9 September 2022]. Available from: https://www.ncpro.org/pubs/2020-encpt-en/page-055
- Academy of Nutrition and Dietetics. Nutrition Terminology Reference Manual (eNCPT): Dietetics Language for Nutrition Care. NCP Step 4: Monitoring and Evaluation. 2020. [Internet]. [cited 9 September 2022]. Available from: https://www.ncpro.org/pubs/2020-encpt-en/page-015a
- ASCIA Website. [Internet]. [cited 9 September 2022]. Available from: https://www.allergy.org.au/images/stories/anaphylaxis/lists/ASCIA_HP_Checklist_Anaphylaxis_Adrenaline_Prescribers_2021.pdf
- Guide for Milk Substitutes in Cow’s Milk Allergy [Internet]. [cited 1 December 2022]. Available from: https://www.allergy.org.au/images/stories/pospapers/ASCIA_HP_Guide_CMA_Milk_Substitutes_2022.pdf
- NHMRC. Nutrient Reference Values. [Internet]. [cited 1 December 2022]. Available from: https://www.eatforhealth.gov.au/nutrient-reference-values
- The GP Infant Feeding Network. The Milk Allergy in Primary Care (MAP) Guideline 2019. [Internet]. [cited 1 December 2022]. Available from: https://gpifn.org.uk/imap/
Eosinophilic oesophagitis (EoE) is a chronic inflammatory disease characterised by eosinophil-rich inflammation which causes symptoms of oesophageal dysfunction.(1) If EoE is not treated oesophageal remodeling, rigidity and luminal narrowing can occur resulting in fibrosis and strictures.(1)
The prevalence of EoE has increased since it was first described 30 years ago. There is now up to 12.8 per 100 000 new cases annually.(2) EoE is non-IgE-mediated and is a T-helper-2 mediated response to food allergens.(2) Diagnosis is made by endoscopy with biopsies indicating eosinophil density of >15 per high-powered field.
Clinical presentation varies with different ages. Almost half of children diagnosed with EoE have coexisting allergic rhinitis, asthma, eczema and/or IgE-mediated food allergy.(3)
References — EOE
- Gonsalves NP, Aceves SS. Diagnosis and treatment of eosinophilic esophagitis. J Allergy Clin Immunol. 2020 Jan;145(1):1-7.
- Chang JW, Haller E, Dellon ES. Dietary Management of Eosinophilic Esophagitis: Man Versus Food or Food Versus Man? Gastroenterol Clin North Am. 2021 Mar;50(1):59-75.
- Munoz-Persy M, Lucendo AJ. Treatment of eosinophilic esophagitis in the pediatric patient: an evidence-based approach. Eur J Pediatr. 2018 May;177(5):649-663.
- Academy of Nutrition and Dietetics. Nutrition Terminology Reference Manual (eNCPT): Dietetics Language for Nutrition Care. NCP Step 1: Nutrition Assessment. 2020. [Internet]. [cited 9 September 2022]. Available from: https://www.ncpro.org/pubs/2020-encpt-en/page-015
- Academy of Nutrition and Dietetics. Nutrition Terminology Reference Manual (eNCPT): Dietetics Language for Nutrition Care. NCP Step 2: Nutrition Diagnosis. 2020. [Internet]. [cited 9 September 2022]. Available from: https://www.ncpro.org/pubs/2020-encpt-en/page-036
- Academy of Nutrition and Dietetics. Nutrition Terminology Reference Manual (eNCPT): Dietetics Language for Nutrition Care. NCP Step 3: Nutrition Intervention. 2020. [Internet]. [cited9 September 2022]. Available from: https://www.ncpro.org/pubs/2020-encpt-en/page-055
- Dellon ES, Liacouras CA, Molina-Infante J, Furuta GT, et al. Updated International Consensus Diagnostic Criteria for Eosinophilic Esophagitis: Proceedings of the AGREE Conference. Gastroenterology. 2018 Oct;155(4):1022-1033.e10.
- Kelly KJ, Lazenby AJ, Rowe PC, et al. Eosinophilic esophagitis attributed to gastroesophageal reflux: improvement with an amino acid-based formula. Gastroenterology 1995;109:1503–12.
- Molina-Infante J, Arias A, Barrio J, Rodriguez-Sanchez J, Sanchez-Cazalilla M, Lucendo AJ (2014) Four-food group elimination diet for adult eosinophilic esophagitis: a prospective multicenter study. J Allergy Clin Immunol 134:1093–1099
- Kliewer KL, Cassin AM, Venter C. Dietary Therapy for Eosinophilic Esophagitis: Elimination and Reintroduction. Clin Rev Allergy Immunol. 2018 Aug;55(1):70-87.
Mixed and Cell-mediated Allergies
- Eosinophilic Gastroenteritis - involves eosinophilic infiltration of various aspects of the gastrointestinal tract, resulting in a range of symptoms such as abdominal pain and malabsorption.
- Atopic Dermatitis - a chronic skin condition exacerbated by food allergies, involving both IgE and non-IgE-mediated mechanisms.
Management Strategy for Food Allergy
Medical Nutrition Therapy
MNT Supporting Food Allergy DIagnosis
MNT in Managing Food Allergy
Aims of Medical Nutrition Therapy
- To eliminate foods proven to cause an allergic reaction while maintaining a nutritionally adequate diet.
- To assist families in maintaining strict adherence to an allergen-free diet.
- To improve nutritional intake, growth and development
- To prevent long-term complications
Evolving Recommendations for Preventing Food Allergies
Dietitians must stay informed about the rapidly evolving guidelines for preventing and treating food allergies. Not long ago, the prevailing recommendation was for infants at high risk of developing food allergies to avoid foods likely to cause allergic reactions. Current strategies, particularly for specific allergens like peanuts, now advocate for early introduction protocols, which have shown to be more effective in preventing the development of allergies. This shift underscores the importance of staying current with emerging research and updated clinical guidelines. All common allergenic food are introduced as part of a variety of solid foods in the first 12 months of life.(5)
The Dual Allergen Exposure Hypothesis
The dual allergen exposure hypothesis posits that low-dose cutaneous exposure, particularly when the skin barrier is compromised, leads to sensitization, while oral exposure promotes tolerance. This hypothesis is supported by substantial evidence and has influenced global changes in infant feeding guidelines.(4)
Anaphylaxis Management
Anaphylaxis must be treated immediately with an adrenaline auto-injector and urgent transport to a hospital. All individuals at risk of anaphylaxis should:
- Be familiar with the emergency procedure
- Have an Australasian Society of Clinical Allergy and Immunology (ASCIA) Action Plan or Food Allergy Research & Education (FARE) for Anaphylaxis completed by their doctor
- Carry an adrenaline auto-injector and understand its use
Death from anaphylaxis is rare. However, it is important to note a history of previously mild reaction does not indicate the severity level of a subsequent reaction. Risk is increased by:
- Delayed or no administration of adrenaline
- Upright posture during anaphylaxis
- Age: Adolescent to young adult
- Presence of co-factors
- Cofactors that may influence the severity of reactions are:
- Poorly controlled asthma
- Exercise
- Menses
- Acute illness
- Nonsteroidal anti-inflammatory drugs (NSAIDS)
- Alcohol
- Sleep deprivation
- Medication: B-blockers, Ace inhibitors
- Reliance on oral antihistamine alone to treat symptoms
- Cofactors that may influence the severity of reactions are:
1. Adapted from National Academy of Sciences, Engineering, and Medicine. Finding a path to safety in food allergy: Assessment of the Global burden, causes, prevention, management, and public policy. Washington DC, National Academies Press; 2017
Interdisciplinary Roles (insert table from Evas article)
TRANSITION TO CASE SPECIFIC ALLERGY INFORMATION FROM THIS POINT FORWARD

